When Ruth Iliya was diagnosed with Tuberculosis (TB) in 2021 at the age of 17, she felt as though her world was crumbling around her.
It all began with a single cough on a quiet Sunday evening, which persisted relentlessly for several weeks. Concerned about her persistent cough coupled with symptoms like weakness and weight loss, her neighbour urged her to seek medical attention, recognizing that this was no ordinary cough.
On getting to the health facility, Ms Iliya was diagnosed with TB and promptly referred to the Wuse General Hospital where she was placed on treatment for some time with no significant improvement.
Recounting her ordeal battling one of the world’s deadliest infectious diseases, she said “It was a very difficult time for me and my family because the treatment I was receiving at the early stage of diagnosis was not working well. I was very ill and almost unrecognizable.

“After months of no significant improvement, I was referred to Abubakar Tafawa Balewa University Teaching Hospital (ATBUTH) in Bauchi state where I was diagnosed with serious Drug-Resistant Tuberculosis (DR-TB),” she said.
Although the diagnosis came as a nightmare to Ms Iliya, she found a glimmer of relief when the doctor assured her that with proper medication, she would get well within few months.
“The doctor and other persons there at the time mentioned that I was the first patient to be placed on a particular type of TB treatment and they assured me of recovering fully,” she said.
An infectious disease
TB, an airborne disease which spreads via the inhalation of droplets primarily from the coughs of infected people — is one of the world’s deadliest infectious diseases, claiming 1.3 million lives in 2022.
According to the World Health Organization (WHO), an estimated 10.6 million people fell ill with TB worldwide in 2022, including 5.8 million men, 3.5 million women and 1.3 million children.

Nigeria, Africa’s most populous nation ranks first in Africa and sixth in the world, accounting for about 4.6 per cent of the global TB burden.
In 2022, Nigeria accounted for 479,000 (19 per cent) of the approximately 2.4 million cases of TB recorded in the Africa region. Out of the 424,000 TB-related deaths in Africa same year, 97,900 (23 per cent) occurred in Nigeria.
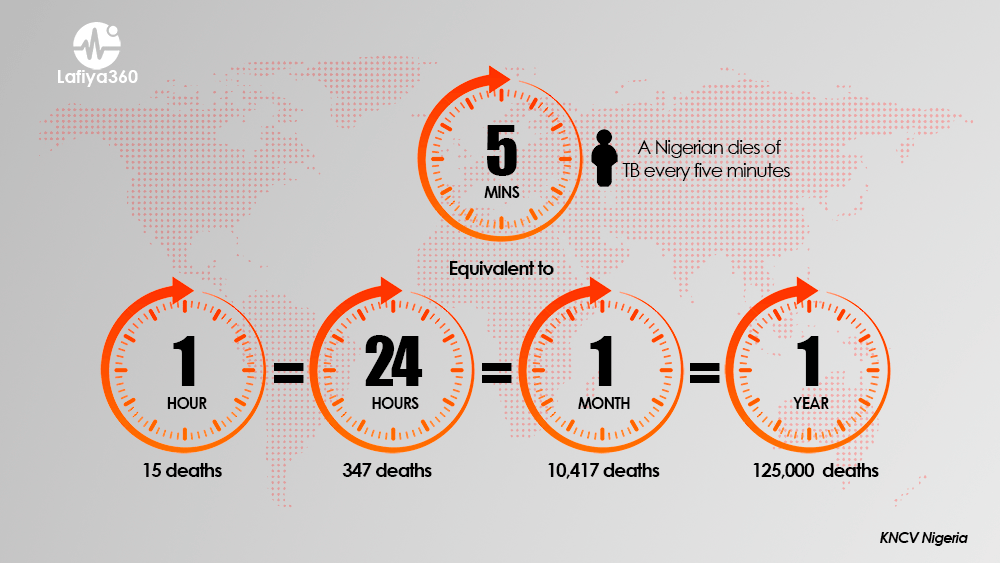
According to KNCV Nigeria, an estimated 15 Nigerians die each hour due to TB, equivalent to about 347 deaths daily, 10,417 monthly and 125,000 in a year.
The HIV epidemic in Nigeria has also contributed to the rise of TB cases, as HIV weakens immune systems and heightens the risk of contracting active TB infection.
Tackling TB
Although, TB is one of the world’s deadliest infectious diseases, a specific combination of antibiotics can cure the infection within four to six months for majority of persons. However, these drugs do not work for people with Drug-Resistant Tuberculosis (DR-TB).

The Deputy Director, National TB, Buruli ulcer, Leprosy Control Programme, (NTBLCP) Federal Ministry of Health, Dr Adesigbin Clement, said DR-TB occurs when the TB bacteria become resistant to at least one of the first-line existing TB medications.
Dr Clement said, “If a patient fails to take TB medication as prescribed, the germs learn to survive around the medication when it is introduced in the future, that is how resistance develops because the germs now learn how to resist the medication.”
DR-TB is classified into two main categories: Multidrug-resistant TB (MDR-TB), which arises when bacteria exhibit resistance to at least two potent first-line anti-TB medications, such as isoniazid and rifampin, and extensively drug-resistant TB (XDR-TB), an even more resistant form occurring when certain TB strains develop resistance not only to first-line medications but also to some second-line medications.
DR-TB, in any of its forms, can be contracted from a person carrying that specific type of TB or can develop if a patient does not finish or consistently take their TB medication, allowing resistance to one or more of the drugs.
Data from KNCV Nigeria shows that in 2021 about 2,975 DR-TB cases were diagnosed out of an estimated 21,000 cases in the country, leaving more than 80 per cent of the resistant cases missing.
The WHO identifies DR-TB as a major contributor to antimicrobial resistance worldwide, posing a substantial threat to public health. Annually, about half a million people fall ill with DR-TB globally.
Groundbreaking regimen
Ms Iliya is the first TB patient in Nigeria to be treated with a new, ground-breaking DR-TB treatment called the BPaL regimen. The regimen, consisting of the drugs bedaquiline, pretomanid, and linezolid was developed by TB Alliance and is implemented in Nigeria by the National TB Programme (NTP), with support from KNCV Tuberculosis Foundation (KNCV).
The regimen, which was approved by the US Food & Drug Administration (FDA) in 2019, boosts shorter treatment duration, lower pill burden on patients and high efficacy.
Before this advancement, treatment for DR-TB typically extends for a minimum of 12 months and could last up to 20 months. This treatment regimen involved the administration of injectable drugs, which were notably painful, often resulting in numerous side effects for patients, including hearing loss.

”With the BPaL regimen, a patient will only undergo an all-oral treatment for about six months with no severe side effects,” the Executive Director for KNCV Nigeria, Dr Bethrand Odume said.
Dr Odume in a chat with Lafiya360 said the treatment for DR-TB has evolved, suggesting a promising indication that with the appropriate tools, the world can effectively combat TB.
“The good news now is that the treatment for DR-TB occurs in the community because there is an evolution in science based on scientific evidence,” he said.
“At KNCV, we have worked with the national TB programme to introduce the BPaL option which is a shorter treatment regimen for DR-TB patients. We have also gotten a good outcome from the treatment where people adhere to this medication religiously.”
The WHO said BPaL will enable much better treatment and treatment outcomes for people with DR-TB, while also helping health systems to provide care for more people.
The effectiveness of the BPaL regimen is also evident in Rose Shuaib, a resident of Suleja in Niger state. Ms Shuaib, a survivor of MDR-TB said she is grateful and happy to be alive. “If anyone had told me I would survive TB, I wouldn’t believe it but see how healthy I look now,” she said.
Recalling her treatment experience, Ms Shuaib highlighted the significance of medical advancements, noting that without them, her treatment duration could have extended to nearly two years.
The Deputy Director of NTBLCP, Dr Clement said Nigeria piloted the BPaL treatment in some states to gain deeper insights to help make informed decisions.
He said the government has been able to scale up the BPaL treatment across the country so far. “So every state is already implementing BPaL, hence every MDR-TB patient diagnosed now is placed on this treatment.”
Funding challenges persist
Despite the advancement represented by the introduction of the BPaL regimen for TB treatment in Nigeria, the persistent challenges of funding for TB remain a pressing issue in the country.
Several health experts and TB advocates point to inadequate funding and delays in the timely release of budgeted funds as major contributors to the failure to eliminate the disease.
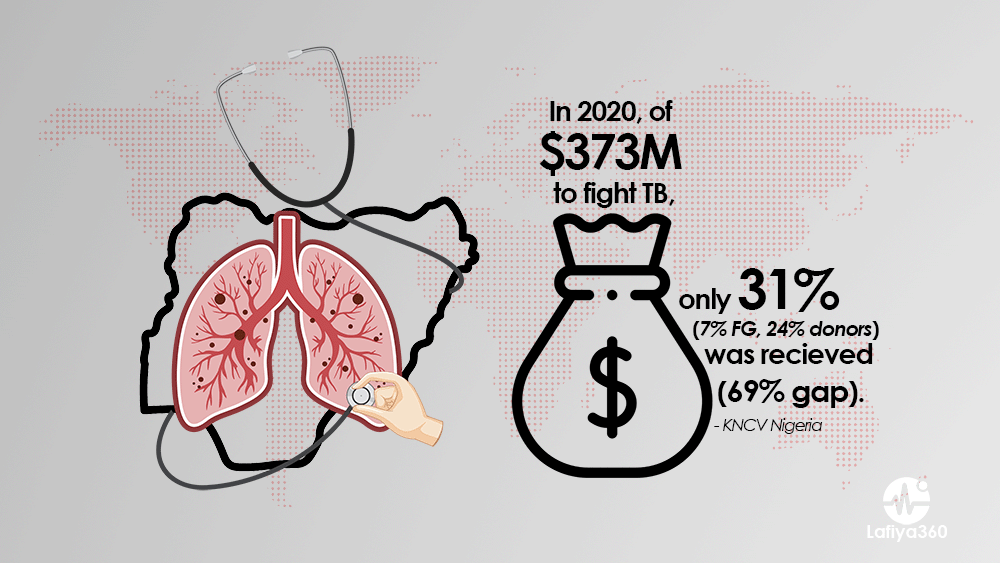
Out of the required $373 million for TB control in Nigeria in 2020, only 31 per cent was accessible to all entities involved in TB control activities (7 per cent domestic and 24 per cent donor funds), leaving a significant funding gap of 69 per cent.
“Without political will and adequate resources at all levels, we cannot control TB,” Dr Amos Omoniyi, the National Programme Officer for TB, WHO said.
Dr Omoniyi highlighted Nigeria’s significant funding gap for TB, noting that approximately 70 per cent of the TB budget remains unfunded. He said this shortfall severely limits the ability to extend TB services to all corners of the community, with a substantial portion of the remaining 30 per cent reliant on donor funding.
He said the implications of this funding gap are far-reaching, as TB services are unable to reach as many individuals as necessary. “Additionally, only half of the health facilities in the country are equipped to provide TB services due to resource constraints.”
“A lot of cases are still being missed and most communities do not have access to treatment centres because there are no funds to support such centres. The Nigerian government needs to step up and fund TB programmes,” he said.
Limited diagnostic tools, low awareness
Health experts have emphasized that the limited availability of diagnostic tools for TB presents significant obstacles to efforts aimed at eliminating the disease.
The experts reiterated that without access to accurate and efficient diagnostic tools, there is a heightened risk of underdiagnosis and misdiagnosis, leading to delayed treatment and increased transmission rates.
Dr Omoniyi revealed that only 48 per cent of LGAs in the country possess the GeneXpert machine recommended by WHO for TB diagnosis. Consequently, individuals in 52 per cent of LGAs must travel to other areas to access TB services, further exacerbating the challenges in combating the disease.
“By expanding access to reliable diagnostic tools, healthcare providers can promptly identify TB cases, initiate appropriate treatment, and prevent further transmission,” he said.
In a message to commemorate the 2024 World TB Day, WHO regional director for Africa, Dr Matshidiso Moeti said challenges such as delayed diagnosis, limited access to new tools and technologies, and the ongoing threat of MDR-TB require continued vigilance and sustained efforts.
Dr Moeti said health leaders must intensify their commitment to strengthening health systems, ensuring equitable access to TB care, and scaling up innovative interventions. She highlighted that investing in research and developing new tools, including vaccines and improved diagnostics, is essential to accelerate progress.
“Furthermore, countries must prioritize addressing the social determinants of TB, such as poverty, inequality, and limited access to healthcare, to achieve sustainable outcomes,” she said.
To address the issue of limited diagnostic tools, Olayide Akanni, the National Coordinator, Civil Society for the Eradication of TB in Nigeria (TBNetwork) said there are plans to conduct a national survey to determine the actual burden of DR-TB in the country.
Ms Akanni said once the national programme concludes this survey, it will provide comprehensive insights into the true burden of TB in Nigeria, pinpointing areas with the highest prevalence and guiding optimal deployment of diagnostic tools and services to those locations.
“It would be pointless to have one machine for diagnosis of MDR-TB in a place where data shows about 300 or more cases, meanwhile there are places with very few cases and lots of machines available there,” she said.
Another key barrier to eliminating TB is lack of access to information, according to Dr Odume, the Executive Director of KNCV Nigeria.
Dr Odume said various research has consistently shown that a significant portion of individuals, particularly those residing in rural areas, possess insufficient knowledge regarding TB. Many health professionals are also of the opinion that this widespread lack of understanding about TB significantly hampers the identification and presentation of cases.
Furthermore, these experts emphasize that if awareness regarding TB remains deficient, the goal of eliminating the disease will become increasingly challenging.
“Once people are aware of TB, its symptoms and the danger it poses to human health, they will be quick to visit the closest health facility once the need arises,” Dr Odume said.
Ms Iliya, the first TB patient to receive the BPaL regimen for DR-TB initially had little knowledge about TB. However, after her successful recovery, she has transformed into a TB advocate, actively raising awareness about TB and its consequences within her community.